Diabetes is a disease that affects 30.3 million Americans according to the National Diabetes Statistics Report in 2017. The same report indicated that 84.1 million people have prediabetes that, if left untreated, may lead to Type II diabetes within five years. Patients who have been diagnosed with diabetes are encouraged to check their blood sugar regularly and to make adjustments as needed to maintain normal blood sugar levels through diet, medication, and exercise.
What is Diabetes
Diabetes occurs when production of insulin is inadequate or when the body does not respond properly when insulin is released. Diabetics experience fluctuations in blood sugar which impact the function of kidneys, heart, nerves, eyes, and other parts of the body. There are four different kinds of diabetes (prediabetes, gestational, Type I, and Type II). Diabetes is more prevalent in adults, yet juvenile diabetes is on the rise.
Systemic Symptoms
Early diagnosis and treatment for diabetes is crucial to maintain systemic and oral health. Symptoms associated with diabetes include excessive thirst, frequent urination, weight loss, and fatigue. If you experience one or more of these symptoms and have not seen a healthcare provider recently, we encourage you to visit your primary provider for an evaluation.
Oral Symptoms
Oral symptoms of diabetes include xerostomia (dry mouth), increased risk of cavities and thrush (oral candidiasis), delayed wound healing, and halitosis (bad breath). Patients may seek dental and medical treatment due to the discomfort associated with xerostomia. The exact cause of xerostomia in diabetics is unknown; however, it may be caused by high blood glucose levels. When oral disease is present in diabetics, early treatment is recommended to avoid more invasive treatments at a later time.
Coorelation with Periodontal Disease
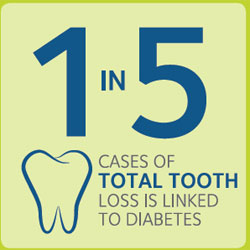 Extensive research has been done on the effects of diabetes on oral health, and indicates a relationship between periodontal disease and diabetes. Periodontal disease is one of the most concerning oral manifestations of diabetes because of the long term effects of early tooth loss and difficulty chewing. Inflammation, poor immune response, and alveolar (bone that holds the teeth) bone loss are all contributing factors to more advanced gum disease for diabetics.
Extensive research has been done on the effects of diabetes on oral health, and indicates a relationship between periodontal disease and diabetes. Periodontal disease is one of the most concerning oral manifestations of diabetes because of the long term effects of early tooth loss and difficulty chewing. Inflammation, poor immune response, and alveolar (bone that holds the teeth) bone loss are all contributing factors to more advanced gum disease for diabetics.
When a patient is diagnosed with and receives proper treatment for periodontal disease, their glycemic (blood sugar) control also improves. An article published in the Journal of Clinical Periodontology states:
“Many studies have shown that periodontal therapy improves glycemic control (blood sugar control) with diabetes. Periodontal therapy in diabetic patients improved glycemic control by 17.1% compared to 6.7% in diabetic patients who did not receive periodontal therapy.”
Periodontal Examinations
A thorough periodontal exam includes both dental radiographs and periodontal evaluations. These are fundamental to a proper diagnosis of periodontal disease. If your dentist informs you of periodontal disease or gum disease, you will receive specific treatment recommendations to target the disease. Scaling and root planing, laser therapy, antibiotic therapy, and surgical therapy may be included depending on the stage of periodontal disease.
Necessity of Regular Dental Visits
Regular dental visits are recommended to evaluate the presence or absence of oral infections, cavities, and periodontal disease. Based on the findings in your oral exam, your dentist may encourage you to return for more frequent gum treatment (periodontal maintenance visits) to minimize the progression of periodontal disease. In addition, after a thorough dental exam, your dentist may recommend a visit to your medical doctor for further evaluation and or testing for diabetes. If you have been diagnosed with diabetes by your medical professional, he/she will likely recommend regular visits to the dentist to maintain healthy gums and teeth.
Contact Us
Call Hogan Family Dental at (406) 234-2926 to learn more or to schedule your regular exam. We are here to help.